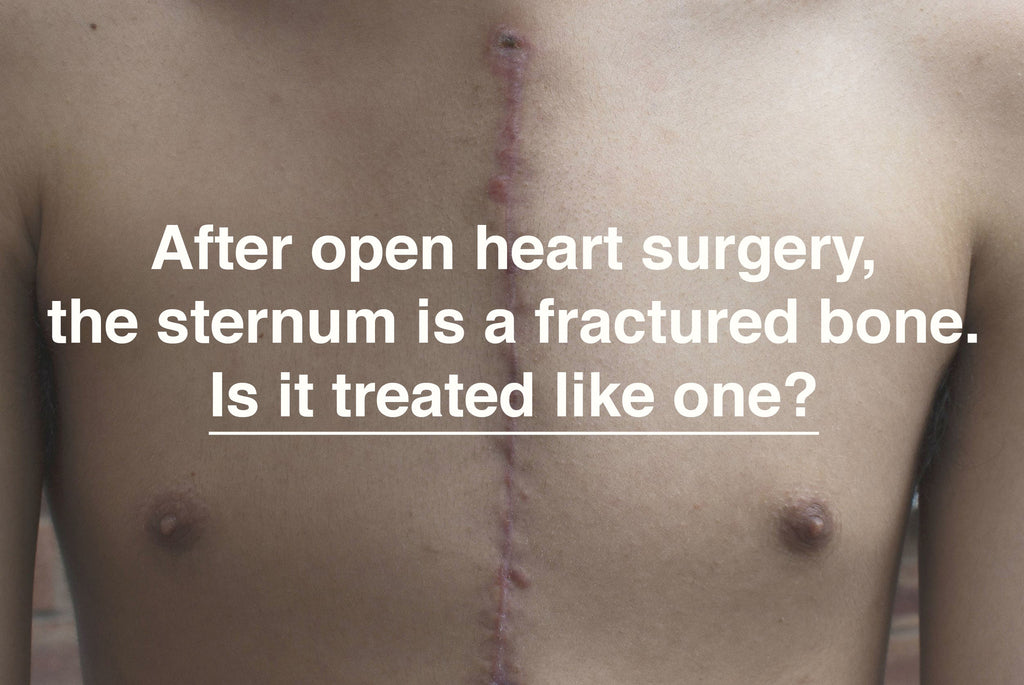
Once heart surgery has been performed and the chest has been closed, in regards to the healing of the sternum, the patient is an orthopedic patient. Do the commonly used techniques for post-sternotomy bone fixation and fracture management follow the generally recognized principles of fracture treatment that are followed in other types of orthopedic repairs? To examine how sternal fracture repair compares to the techniques used in other orthopedic repairs, it’s instructive to return to basics and to review the principles of bone fracture treatment.

How are bone fractures treated?
The 4 basic principles of bone fracture management, as defined by the AO (Arbeitsgemeinschaft für Osteosynthesefragen / Association for the Study of Internal Fixation), have changed little since first published in the early 1960s.1 The current version of the principles of fracture management is as follows:
- Anatomic reduction of the fracture fragments (realigning the pieces of the broken bone back to their correct anatomical position)
- Fracture fixation, providing absolute or relative stability, to fulfill biomechanical demands (hold the bone in place with enough stability to allow it to heal and enough flexibility for the bone to perform its anatomical function)
- Preserve blood supply to the injured area (both the injured bone and surrounding soft tissues)
- Early and safe mobilization and rehabilitation of the injured part and the patient as a whole.
"The internal wire fixation is often supplemented by secondary external fixation, in the form of casting or splinting"
When the internal mammary artery is used as a coronary artery bypass graft, the blood supply to the thoracic wall, including the sternum, is compromised. While this compromise in blood supply to the fractured bone is critical to the surgery, it does constitute a “violation” of the third principle of fracture management and likely affects the bone and soft tissue healing time. This necessary “violation” may make adherence to the remaining three principles of fracture management more important.
At this time, the primary method of fracture fixation post-sternotomy remains the use of steel wires to close the sternum.2 Wires resist changes in alignment but do not provide rigid fixation and therefore do not provide absolute stability to the sternum. When wires are used as the primary form of fixation in other orthopedic surgeries, the internal wire fixation is often supplemented by secondary external fixation, in the form of casting or splinting.
"In the case of the sternum, the biomechanical forces the repaired sternal fracture must withstand are significant"
Looking to the principles of AO bone fracture management, it’s necessary to consider the anatomical function of the sternum and the need for the methods of fixation to provide sufficient stability to allow the sternum fixation to hold up to the biomechanical demands of the anatomy. In the case of the sternum, the biomechanical forces the repaired sternal fracture must withstand are significant.
A cough places approximately 60 pounds pressure on the sternum; a sneeze places approximately 90 pounds pressure on the sternum.3 Given the need to cough and perform breathing exercises during the rehabilitation and recovery period, the effects of this pressure must be considered. In many instances in which wire alone is used to provide fixation to the sternum, there is the recognition that additional support is needed during coughing. Patients are often instructed to use a self-hugging maneuver, or to hug a pillow when coughing to provide support against the pressure of the cough force on the fractured sternum.

The efficacy of the pillow as fracture support, however, hasn’t been reported (Read more here). The use of the pillow also seems to potentially be contrary to the fourth principle of bone fracture management, which is “early and safe mobilization and rehabilitation of the injured part and the patient as a whole”. It seems counterintuitive that a patient will be encouraged to be mobile and begin resuming daily activities when he must make use of a pillow to provide sternal support during unanticipated coughs and sneezes. The use of the pillow does not encourage activity and may, in fact, decrease activity, if the act of hugging the pillow decreases pain caused by the pressure of the cough on the sternal fracture. The patient may be encouraged to remain relatively sedentary, in order to stay within reach of the pillow.
Splinting by use of an external brace has been studied and has been shown to significantly reduce sternal separation. Patient-reported pain scores during movement were correlated with the degree of sternal separation, and patients wearing an external brace reported significantly less pain during movement than when using alternative external supports that allowed for greater sternal separation.4 This study suggests that using an external brace as an adjunctive bone fixation device provides additional sternal stability and may promote safer rehabilitation and mobility than the use of wires alone. Given that the wearable external support moves with the patient, unlike the pillow, the brace provides constant splinting support to the patient and may promote mobility and allow for earlier rehabilitation and return to normal activities. Progressive and active rehabilitation activities are necessary to improve a patient’s functional status and pulmonary function post-sternotomy.5
Any external support device used to provide sternal support must be limited to the upper torso; the lower lung lobes and upper abdominal areas should not be covered, such that breathing is not restricted. External stabilization of the sternum may have the additional benefit of encouraging abdominal breathing and engagement of the diaphragm, which may help prevent post-operative pulmonary complications.
"In order to align post-sternotomy care with the accepted best practices of bone fracture management, an external brace should be worn during the post-surgical recovery period."
External splinting of the sternum provides the necessary support to the healing sternum to withstand the biomechanical forces exerted during coughing, reduces pain associated with movement, reduces the sternal gap, and allows the patient to regain mobility and participate in rehabilitative activities. In order to align post-sternotomy care with the accepted best practices of bone fracture management, an external brace should be worn during the post-surgical recovery period.
Sternum non-union
If you are looking for more information on non-union of the sternum, have a look at this other article:
Sternal Non-union - what choices do patients have?
References:
- Ruedi TO, Buckley R, Moran C, eds. AO Principles of Fracture management. 2nd Ed. New York, NY. Thieme Medical Publishers, Inc; 2007.
- Kamiya H, Al-maisary SSA, Akhyari P, Ruhparwar A, Kallenbach K, Lichtenberg A, Karck M. The number of wires for sternal closure has a significant influence on sternal complications in high-risk patients. Interact Cardiovasc Thorac Surg. 2012 October; 15(4): 665–670
- Adams J, et al. Comparison of Force Exerted on the Sternum During a Sneeze Versus During Low-, Moderate-, and High-Intensity Bench Press Resistance Exercise With and Without the Valsalva Maneuver in Healthy Volunteers. American Journal of Cardiology, Volume 113, Issue 6, 1045 – 1048
- El-Ansary D, Waddington G, Adams R. Control of Separation in Sternal Instability by Supportive Devices: A Comparison of an Adjustable Fastening Brace, Compression Garment, and Sports Tape. Arch Phys Med Rehabil 2008;89:1775-81
- Cahalin LP, LaPier TK, Shaw, DK. Sternal Precautions: Is It Time for Change? Precautions versus Restrictions – A Review of Literature and Recommendations for Revision. Cardiopulmonary Physical Therapy Journal Vol 22, No 1 March 2011


13 comments
May 03, 2018 • Posted by Joachim
Hi Frances,
Sorry to hear about the pain you are experiencing. Not knowing what is causing it, we can only recommend that you continue to see your doctors so that they may help you find a cause and solution. Hope you get better soon.
Best regards
Joachim at Qualiteam
May 03, 2018 • Posted by Frances Ferris
I had open heart surgery a year ago. Had a graft on my ascending aorta,& a stent put in my ascending aorta. No problems. Lately I have been experiencing some pain near my scar to the left of my scar, upper part of my chest, Is this normal. Blood pressure good. Oxygen levels good, energy good. Had a cat scan done Jan of this year. Stent looks good, graft looks good. Don’t know where the pain is coming from.
Mar 20, 2017 • Posted by Denise Dickerson
After collecting feedback from several patients who have used QualiBreath they have all felt grateful for having it during recovery period. Even those who didn’t care for it at first all agreed once it was taken off they all wanted it back on asap! Excellent product for open heart recovery!
Leave a comment: