Transcript:
In this presentation we review the clinical evidence for using traditional abdominal binders and present a radical new design which will make binders more comfortable and effective.
There are more than 300 million interventions annually worldwide, which averages 1 intervention for every 25 people. However, in developed countries 1 surgery in 11 people is performed, while just 1 per 339 people in underdeveloped countries. We can therefore expect continued significant growth in major abdominal surgery interventions as underdeveloped countries make progress.
Complication rates and mortality after abdominal surgery are difficult to compare due to the variety of interventions. The overall complication rate has been reported to be 17% within 30 days after surgery. Interestingly 40% of those happen after discharge, and 75% of those within 2 weeks after the patients leave the hospital.
Here are the 10 most common complications after major abdominal surgery. Note that the top 5 relate to infections. Almost a third of all complications are superficial site infections, almost 14% are organ space infections, about 11% involves severe sepsis, close to 10% urinary tract infections, and more than 7% are deep surgical site infections. Wound dehiscence is reported in almost 5% of all complications, followed by deep venous thrombosis, pneumonia, septic shock and pulmonary embolism.
Besides being the most common complication, the incidence of surgical site infections is reported to be between 15 to 25% and it doubles the risk of mortality. With19.5% of all readmissions, surgical site infections are also the most common reason for readmission.
Abdominal wound dehiscence is reported in 0.3% to 3.5% and a mortality rate between 25 and 45%. One study reported that broken sutures and loose knots were the reason in 12% of patients with this complication.
Incisional hernia ranges from 2 to 20% of cases with an overall rate of about 10%, however, this rate increases with time and can be as high as almost 70% after 5 years!
Pulmonary complications are presented in 5 to 40% of cases with a mortality rate of 18% and cause a three-fold rise in costs compared to the other complications.
Last but not least postoperative pain is reported in 10 to 50% of cases. Interestingly all authors reporting on the different postoperative complications agree that all complications most likely are under-estimated.
Major abdominal surgery without complications costs about $10.000. Complications increase the costs significantly. Minor complications almost doubles the cost and major complications more than triples the costs to an average of about $33.000.
In addition readmission rates are significant and reported to be about 11% after 30 days and doubles to more than 23% after 90 days.
Postoperative complications increase the length of stay (LOS) in the hospital, increase mortality and may lead to permanent or chronic problems. Complications also reduce the patient’s quality of life (QoL), and obviously lead to a significant increase in health care costs.
There are many risk factors for getting complications after major abdominal surgery, such as age, obesity, diabetes, smoking, and other diseases. Operative characteristics like emergency procedures and complexity of surgery are risk factors too as well as tension and manipulation of the wound after surgery.
How can complications be prevented? It is important to identify patients at risk and for example prescribe breathing exercises, weight loss and non-smoking before surgery in an attempt to decrease such risk. Of course scrupulous sterile technique must be used, and reduction of surgery time if possible. An antibiotics regime and control of postoperative pain can help to decrease complications, as well as postoperative respiratory exercises and early mobilization. It is also important to use careful manipulation of the tissues around the surgical site to reduce stress on the wound.
It is a balancing act to prevent complications after major abdominal surgeries. On one side stabilization of the abdominal wound is important to prevent wound complications such as dehiscence, infections and hernia formations. On the other side coughing is a necessary activity to clear the lungs for secretions. Yet coughing causes a brief but significant increase in intra-abdominal pressure up to 300 mmHg. And deep breathing, sneezing, laughing and straining have a similar effect. However, surprisingly there are no recommendations established concerning how to stabilize the wound other than by the patients hands or the use of a pillow.
Patients instinctively support their wound by holding their hands against it after any abdominal surgery, and the present guidelines advise to do so or to use a pillow.
At the same time the use of a proper technique to get in and out of bed is one of the most important teachings to patients. They are advised to sit on the edge of the bed and stabilize their wound by the hands. That makes it difficult for patients to safely preserve their balance while standing up when they cannot use their hands, and it means STAFF is needed to help them.
So what is the status of using abdominal binders which obviously is a method to get patients hands liberated?
Although early and progressive mobility is widely accepted as an important aspect of postoperative care, only few studies have systematically investigated the effect of maintained incision support on the postoperative recovery, and the majority of these studies do not identify or even describe the binders. Details such as materials used, degree of elasticity, sizing method, height of binder, degree of compression, and other design characteristics can have a significant effect on how effective or comfortable the binders are. Guidelines and recommendations suggesting the timing, frequency, duration, and intensity of mobilization efforts when using binders are nonexistent in literature.
Compression binders are common and a large selection of commodity binders can easily be purchased. However, they are all very similar and have no distinctive design differences. Many are warm and uncomfortable to wear, and they may crawl or roll up on the body. All commodity binders cannot accommodate drainage tubes or other devices without that staff has to cut holes in the binder material and separate the devices from their connecting appliances, which expose the patient to increased risk of infection.
No adverse effects as a result of using an abdominal binder has been reported in literature and evidence is provided that an abdominal binder can safely be incorporated into treatment and care protocols to prevent complications after major abdominal surgery. In fact most investigators find it justified for patients to use an abdominal binder, but still no clear guidelines for use are given! Therefore binders are mostly used according to physician preferences and practices.
Investigators agree that the potential benefits of binder usage are lower risk of dehiscence, incisional hernia and development of wound hematoma, as well as reduction of pain and fear of pain, improved intestinal function, and increased physical activity.
Early and aggressive mobilization after major abdominal surgery has the potential to prevent respiratory complications, reduce inflammation, increase muscle force, and to promote a quicker return of gastrointestinal function. It also prevents a decrease in functional exercise capacity and facilitates overall recovery. In addition, it improves self-perceived functional status, and the positive outcome associated with mobility has been shown to reduce length of stay and reduction of healthcare cost.
The ERAS society which stands for Enhanced Recovery After Surgery publishes guidelines for professionals and patients to encourage fast track recovery after surgery. Although no adverse effects are documented in relation to binder usage, the advice to patients when coughing is: “try holding your abdomen to reduce the pain” and “take a deep breath and cough using a small blanket or pillow to support your incision”.
ERAS advises patients to get out-of-bed after colon and rectal surgery for two hours on the day of surgery and for six hours every following day until discharge. However, compliance with these targets is reported to be very low. In a multi-institutional ERAS society registry compliance was 48% on the first postoperative day and 28% the following day. This means STAFF is needed to encourage and secure that patients mobilize as early as possible!
Breathing exercises and early mobilization are the foundations of postoperative management after major abdominal surgeries.
An effective abdominal binder may be crucial for wound support and stabilization, pain control, and certainly a safer option for support than the patient's hands alone. An effective binder also provides comfort, decreases pain during activities, and gives a feeling of security and it may prevent dehiscence, infections and hernia.
The status of complications after major abdominal surgeries is that they are still unacceptably high. Even if literature supports there are no adverse effects of using ordinary abdominal binders, they are not used as standard of care. Perhaps one of the reasons are that ordinary binders make it difficult to comply with postoperative activities and enhanced recovery programs both for patients and staff.
These are some of the key factors that led to a complete new and radical design change in abdominal binders.
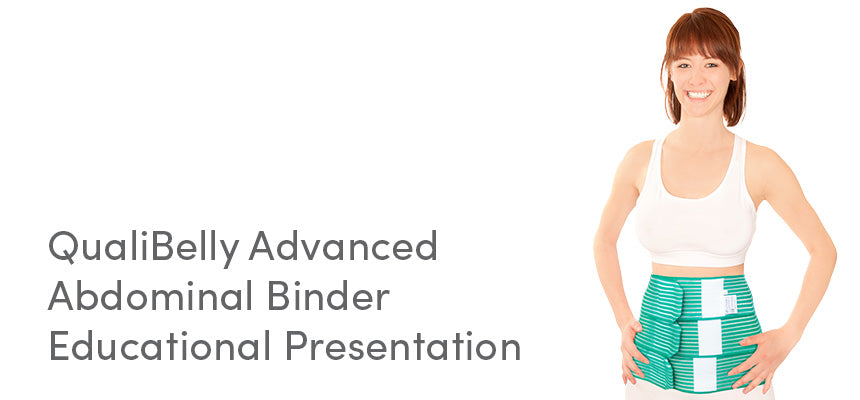
The QualiBelly Advanced is a very different compression binder with advanced features. It has been designed by a nurse to improve functionality and wound inspection for staff and to promote postoperative mobility, security feeling and comfort for the patient. QualiBelly Advanced gives a pleasant, supportive pressure to the abdominal muscles which reduces pain during increased internal abdominal pressures when coughing, sneezing and straining. It also stimulates to have a better posture which improves breathing, and it has important accessories to secure safe line and device organization when patients mobilize.
QualiBelly Advanced consists of 3 overlapping bands that are joined together with a series of small vertical stitches. Each band can be adjusted individually at upper, mid or lower abdominal region to adapt to type of intervention, which increases comfort for the patient.
The design saves time for staff. One person can open one or two of the bands for wound access while the other band(s) remain closed to maintain some degree of support, which makes wound care less painful. And re-closure is possible by just one healthcare person on patients of all body sizes. This will save time and staff needed for wound care.
An important design goal was to make it easier for nurses and to prevent risk of infections. Simply close one band above and the adjoining band below drainage tubes or other devices exiting from the abdomen. No need for cutting holes in the binder and most importantly, no need to separate such systems which decreases the potential for infections. A convenient drainage bottle holder is available to arrange and attach drainage systems directly to the binder without the need for pins or tape. Again saving time and requiring less staff.
QualiBelly Advanced transforms easily into a lower compression binder by folding the upper band down over the middle band. This is useful when sitting down as it relieves pressure on the upper abdominal region and it gives additional support to the lumbar region.
The material is exceptionally light, ventilated and latex-free, and can comfortably be used directly on the skin.
To summarize: The QualiBelly Advanced is a different abdominal binder with numerous advantages other binders do not have and it has the potential to decrease postoperative complications such as abdominal wound dehiscence, infections and hernia formations. It helps patients to have less pain and improved comfort. It increases the sense of security and gives freedom to use hands during activities. It improves posture, promotes deeper and more effective breathing with a potential decrease of pulmonary complications and the related costs of healthcare. Drainage bottles and other devices can be attached directly to patients, and the universal device holder makes it faster, easier and safer to “liberate” the patient for mobilization, saving time and requiring less staff.
Furthermore, it is confirmed in literature that abdominal binders have no negative effect on pulmonary function, and they help to control pain. Patients wearing binders have improved early postoperative mobilization, which is important to avoid complications after surgery, and they promote earlier intestinal activity. Binders help to prevent wound dehiscence and incisional hernia, especially during mobilization and deep breathing exercises. An effective binder can improve comfort, with a better posture and better breathing, and give a feeling of security which have an overall positive psychological effect.
QualiBelly Advanced is designed with the total needs of a postoperative patient and the health care personnel in mind. This advanced abdominal binder promotes less pain and less wound complications, improves wound access and maintains wound support during inspection and care, improves overall comfort for the patient and functional convenience for staff, and it stimulates patients to earlier mobilization in the postoperative period, which may lead to earlier discharge from the hospital with related decrease in costs of health care.
For the references click here: White Paper.
Leave a comment: